Do I have pelvic organ prolapse?
Have you experienced any of the most common symptoms of pelvic organ prolapse (POP)?
Have you experienced any of the most common symptoms of pelvic organ prolapse (POP)?
Pressure or discomfort in the vaginal or pelvic area
Diminished control in the bladder and/or bowels
Pain during intercourse
A bulge near the opening of the vagina
It’s always important to talk to your doctor sooner rather than later when you suspect you may be experiencing symptoms associated with pelvic organ prolapse. There’s no shame in joining the conversation and there is no guilt in putting your health first.
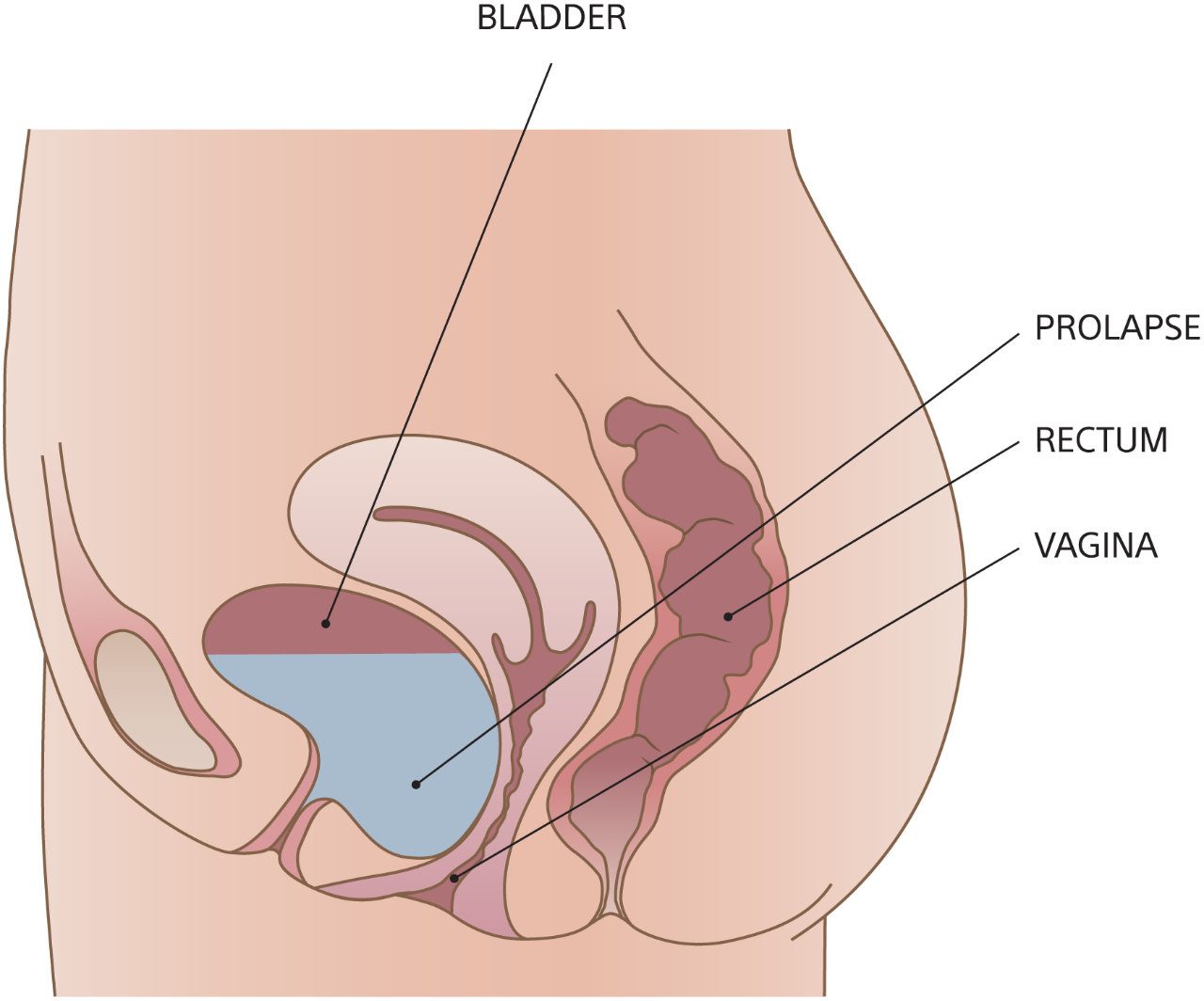
A cystocele forms when the upper vaginal wall loses its support and sinks downward. This allows the bladder to drop. When a cystocele becomes advanced, the bulge may become visible outside the vagina. The symptoms caused by cystoceles can include pressure, slowing of the urinary stream, overactive bladder, and an inability to fully empty the bladder.
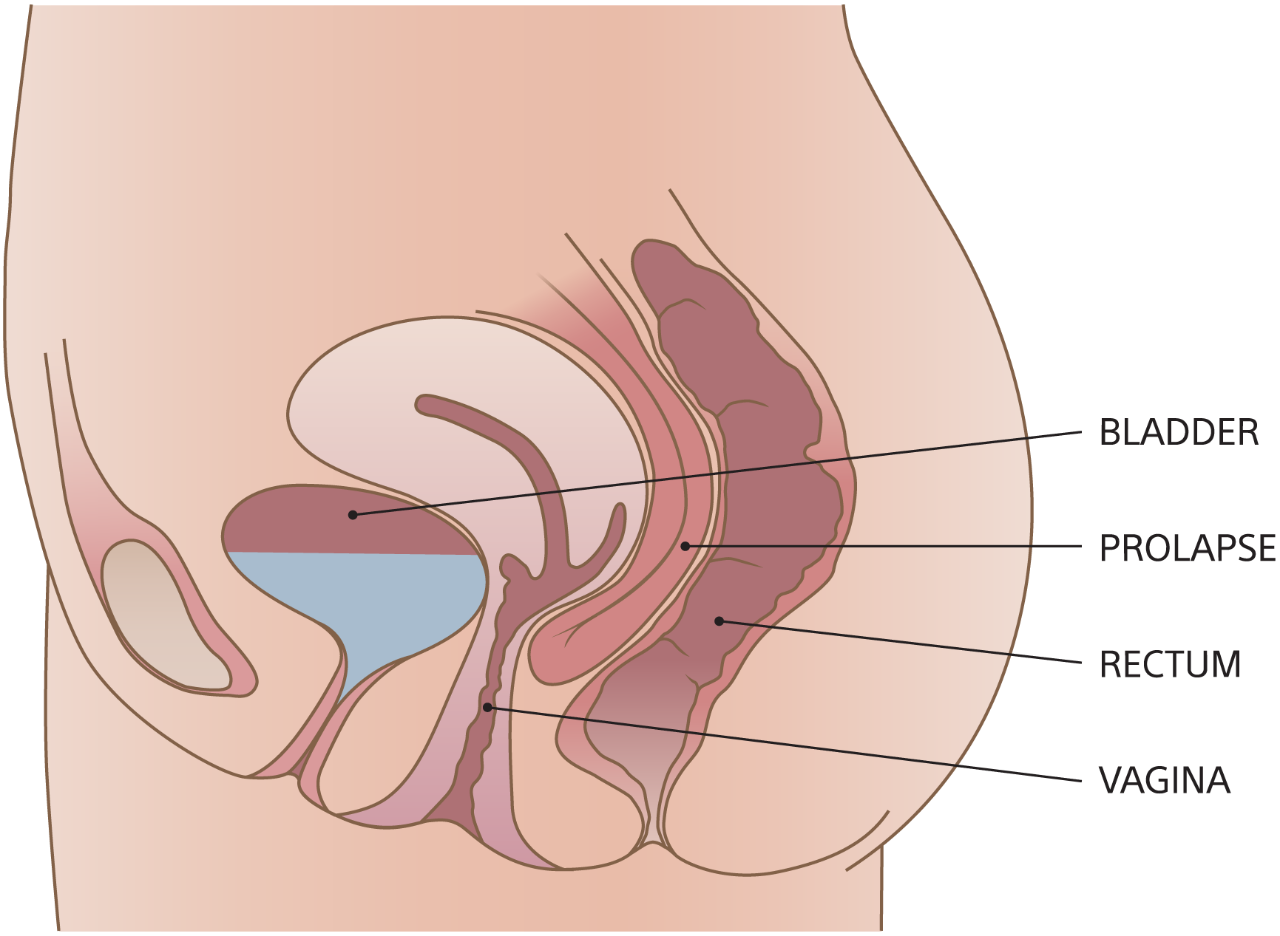
This occurs when the uterine or vaginal support structures holding the upper part of the vagina are weakened. If the uterus is present, this is called “uterine prolapse.” Symptoms include pressure, pain, bladder infections, and difficulty urinating.
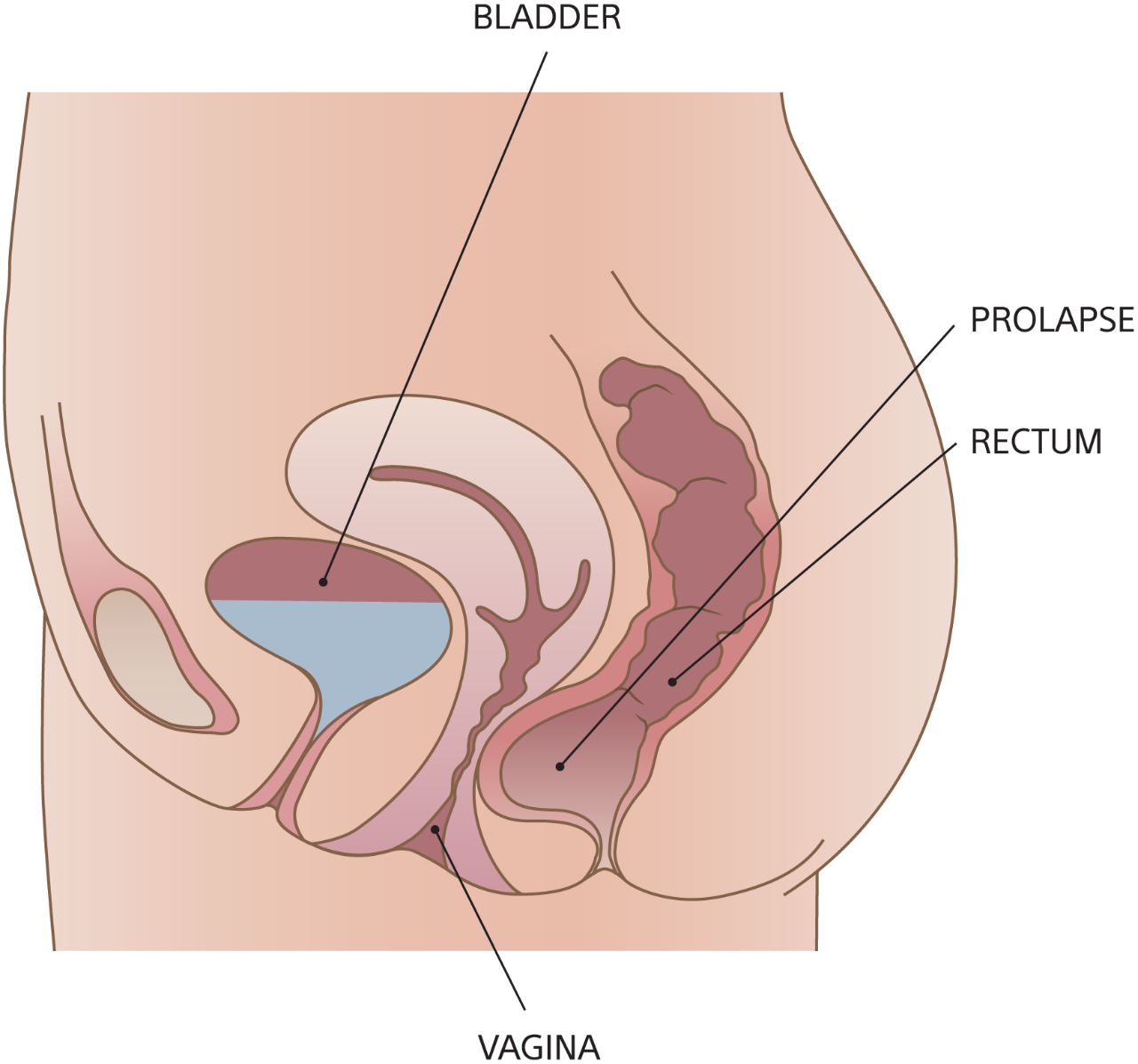
A rectocele forms when the lower vaginal wall loses its support, allowing the rectum to bulge into the vagina. Rectoceles may cause difficulty with bowel movements — including the need to strain more forcefully, a feeling of rectal fullness even after a bowel movement, increased fecal soiling, and incontinence of stool or gas.
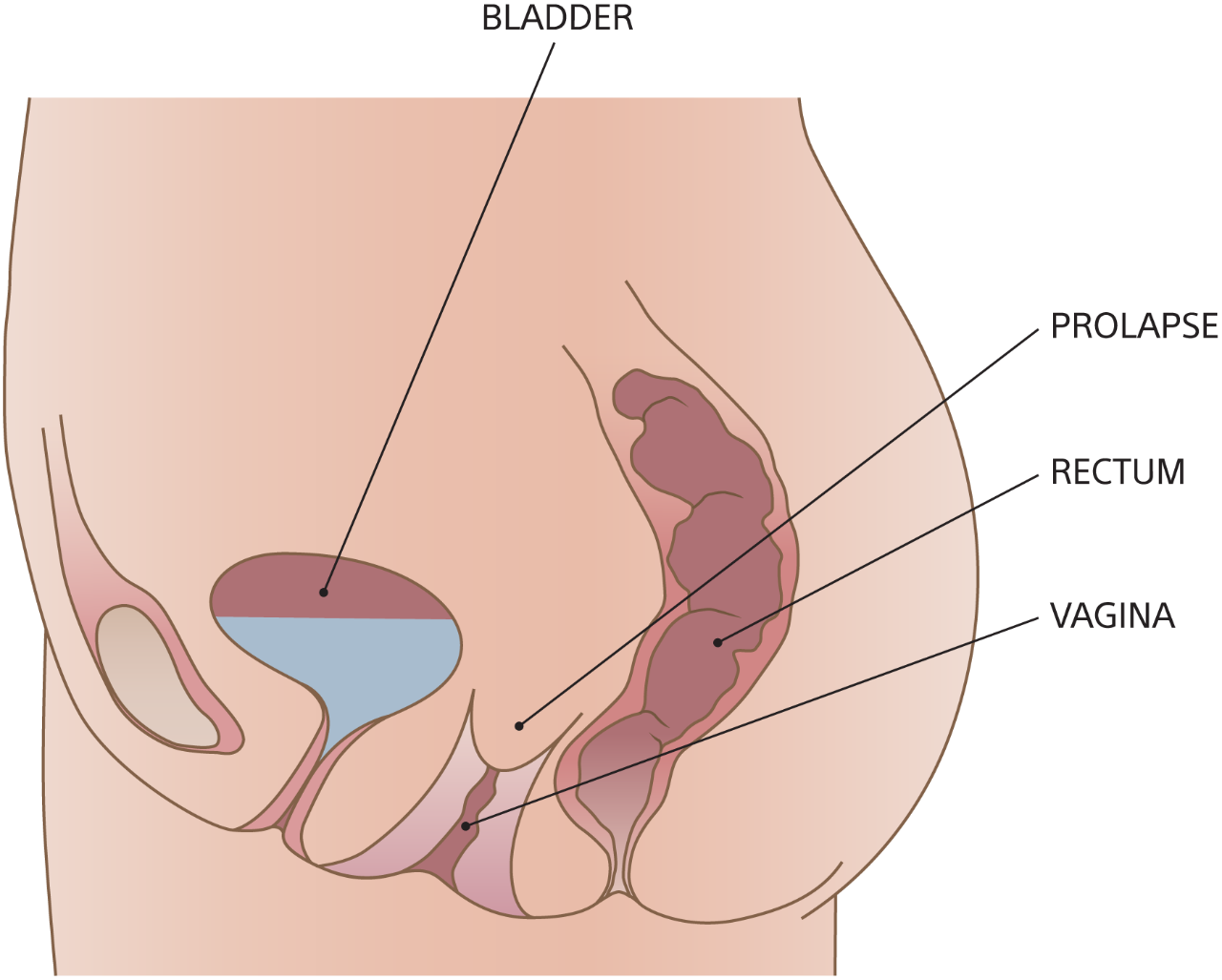
An enterocele typically forms when the small intestine bulges through the top of the vagina after a hysterectomy, but not always. In some women, the intestine may slide between the back of the vagina and the rectum. The symptoms can be vague, including a bearing down pressure in the pelvis and vagina, and perhaps a lower backache.
Pelvic organ prolapse can be treated in several ways, depending on the exact nature and severity of your condition. Talk with your doctor to determine which treatment is right for you.
Boston Scientific is committed to bringing more hope, more health, and more life to women around the world. Learn about Boston Scientific's commitment to women's health